IMC claim ID
IMC claims are sent to health funds via the eClipse network. If it’s necessary to contact a fund to confirm a claim is being processed it’s necessary to provide the fund the servicing doctor’s provider number and the IMC claim ID from the batch handler.
Open the batch handler
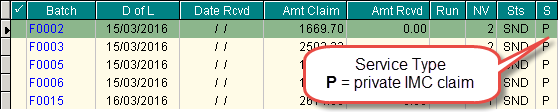
IMC claims are displayed in the batch handler with a service type P.
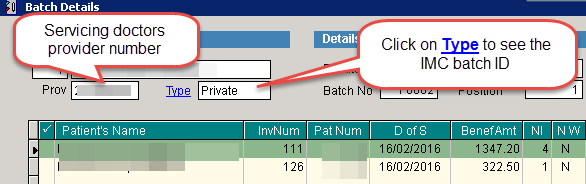
Click on a batch so that it is highlighted and View at the bottom of the screen to open the batch details screen.
Note the servicing doctor’s provider number displayed in the top left corner of the screen. Double click on Type to view the transaction details.
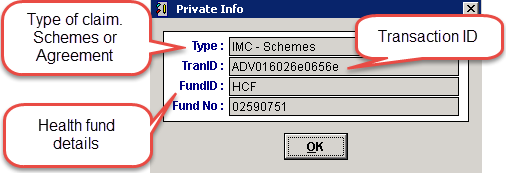
Note the TranID. This is the reference used by the health fund for this claim.
When speaking with the fund quote both the doctors provider number and TranID from this screen for them to check the status of the claim. Depending on the fund it will be necessary to bill claims via Scheme or Agreement. If the wrong claim type is used the claim may be rejected by the health fund.