Batch Status
All claims are separated by service type and this is indicated by the letter M,V,I or P. Usually service type is displayed on the right side of the screen under the heading S
The maximum number of vouchers for each batch can vary depending on the batch type.
| Batch Type | Maximum number of vouchers |
| Medicare | 80 |
| Veterans Affairs | 80 |
| Immunisation | 20 |
| Private | 16 |
| Inpatient Medical Claims | 1 |
Medicare, Veterans Affairs and IMC (In Patient Medical claim) batches have a life cycle from creation to receipt.
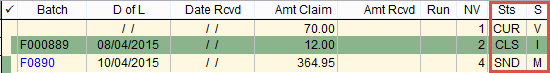
Batch life cycle states (Sts) are
CUR Current batch. New billings are automatically placed in the current batch.
CLS Closed batch. The batch is closed and no new billings can enter the batch but vouchers can be moved out.
SND Batch is assigned and ready to send.
E_S Batch electronically sent or transmitted.
E_R Electronically Received. Acknowledgement that the batch has been received online along with exception and payment file.
If the batch status E_R is black it means that no payment file has been received.
If the batch status E_R is blue it means that the payment file has been received.
RCV Batch has been acknowledged as received and marked as paid in the system.
If you want to know what the different batch states are just hover your mouse over the Sts field in eClaims and a menu will appear explaining the codes.
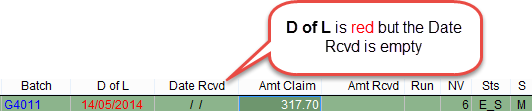
If a batch is displayed in red it indicates that there is an issue. It could be that the batch was sent and no response received for an extended period of time or there is an exception statement.
The example below shows a batch that it overdue to receive payment. The Date of Lodgement was more than 7 days ago and no payment file has been received from Medicare.
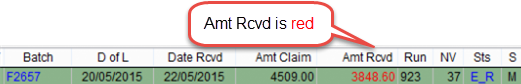
This example shows that a file has been received on the 22nd of May 2015 but the Amt Rcvd (Amount Received) is red. This indicates that Medicare has paid a different amount to the amount claimed. In the example below $4509.00 was claimed and only $3848.60 paid by Medicare. It is necessary to adjust the batch so that the amount claimed is the same as the amount received before the batch can be archived.
For more information refer to How to process payments in the batch handler.