How to process payments in the batch handler
When payments are processed through the batch handler for Medicare or eClipse a file is sent to eClaims noting the amounts paid for each service and any exception or error codes. Typically claims should be processed within a few days but can take up to 7 business days.
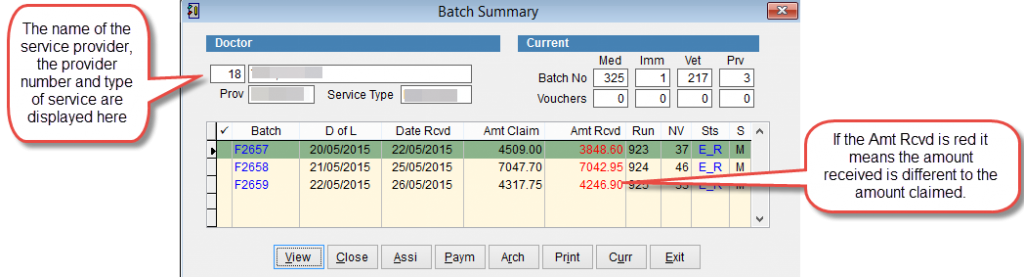
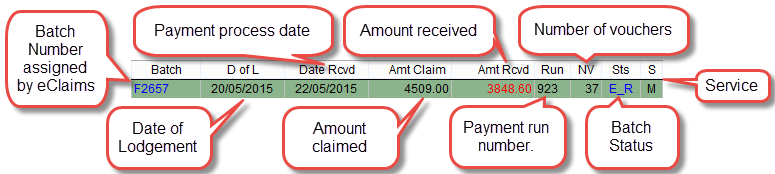
The batch handler has a status (Sts) field to display the where the batch is within the batch life cycle. For more information refer to Batch Status.
For more information on the these fields refer to Batch Summary.
When assessing payment Medicare calculate the amount according to the current MBS Item Number rules. The Amount Received can be more or less than the amount claimed according to these rules. For more information refer to MBS Item Numbers.
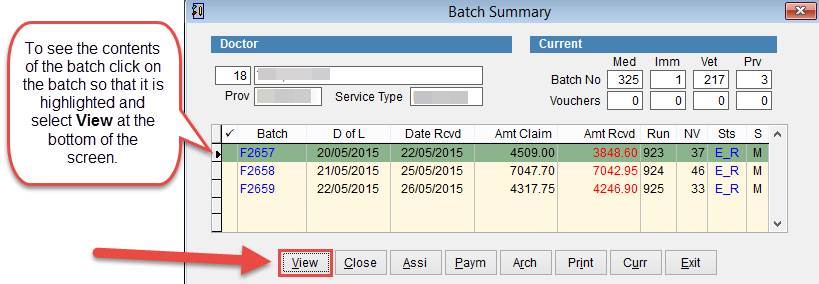
In the example above the amount claimed (Amt Claim) is 4509.00 and the amount received (Amt Rcvd) is 3848.60. The value for amount received is displayed in red because it is not the same as the amount claimed. This is the total for the batch, to see the details click on the batch so that it is highlighted and select View at the bottom of the screen.
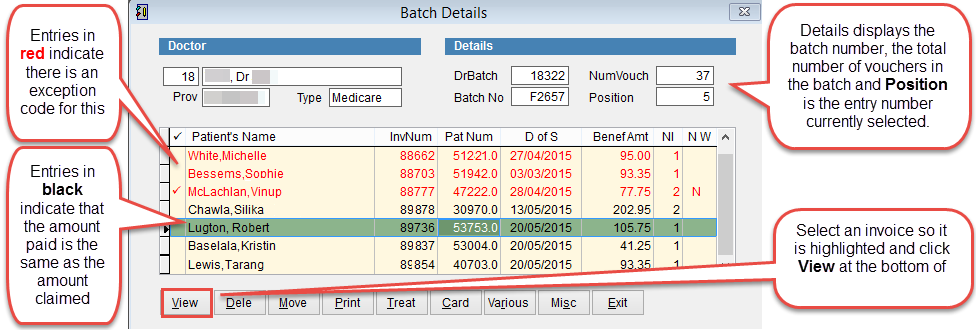
Batch Details displays the patient invoices inside the batch.
Entries in red indicate that the amount paid is different to the amount claimed. Entries in black indicate that the amount paid and the amount claimed are the same.
Before archiving a batch it’s necessary to for all entries to balance.
To see the details of an invoice click on an invoice so that it is highlighted and click View at the bottom of the screen.
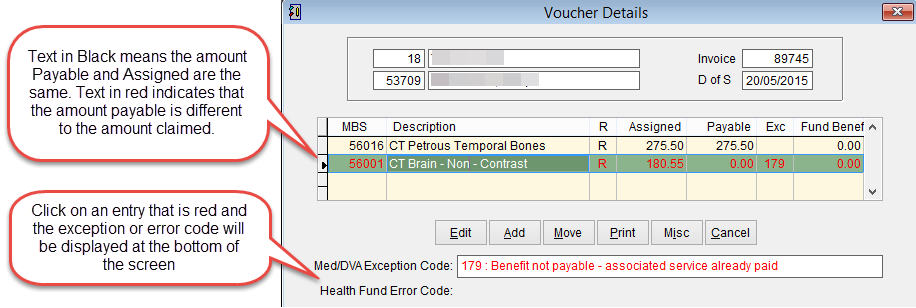
Voucher Details
Voucher Details shows the patient invoice and the amounts paid by either Medicare or the Health Fund and any error or exception codes.
For a list of error and exception code errors refer to Error and Exception Codes
In order to archive the batch it’s necessary for the amount assigned and amount payable to be the same. If lines are red in the voucher details area it is not possible to archive the batch.
Depending on the issue it’s necessary to either adjust the amount payable to be the same as the amount assigned or move the unpaid item out of the batch to another batch and process the claim again.
How to Adjust the Amount Assigned.
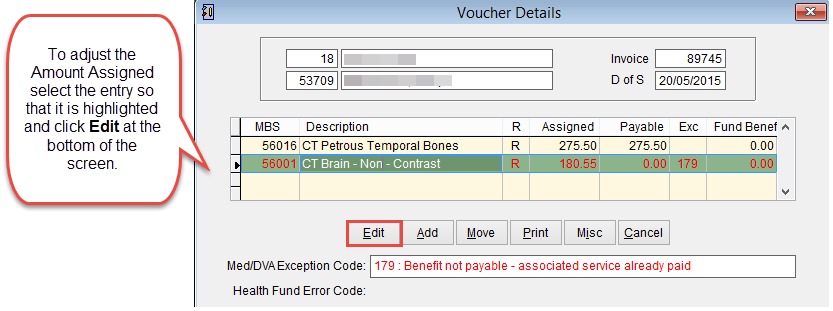
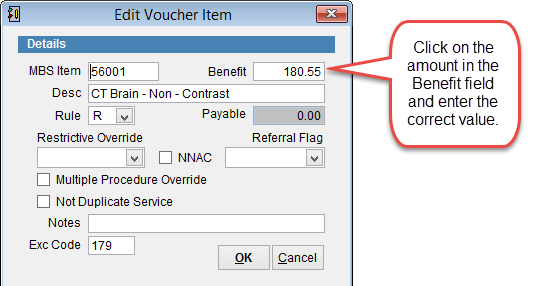
Edit Voucher Item
This screen displays the details of the item within the invoice
To adjust the amount claimed click and modify the amount next to benefit (this is done if the claim had been underpaid).
Click OK to save changes and Cancel to discard changes and return to the previous screen.
In the example above the item had been rejected under exception code 179. If this is correct, you can simply click the Delete button to remove it from the batch. If need be, you can re-bill the service correctly and send it off again for payment.
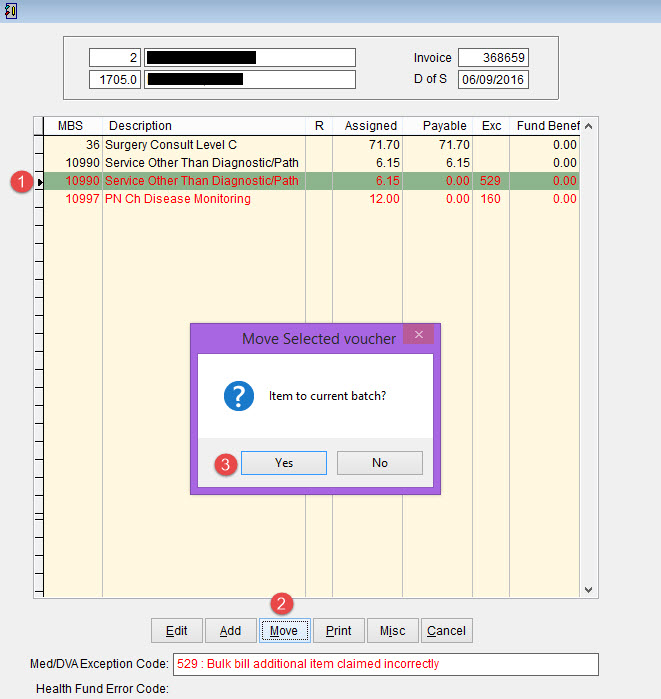
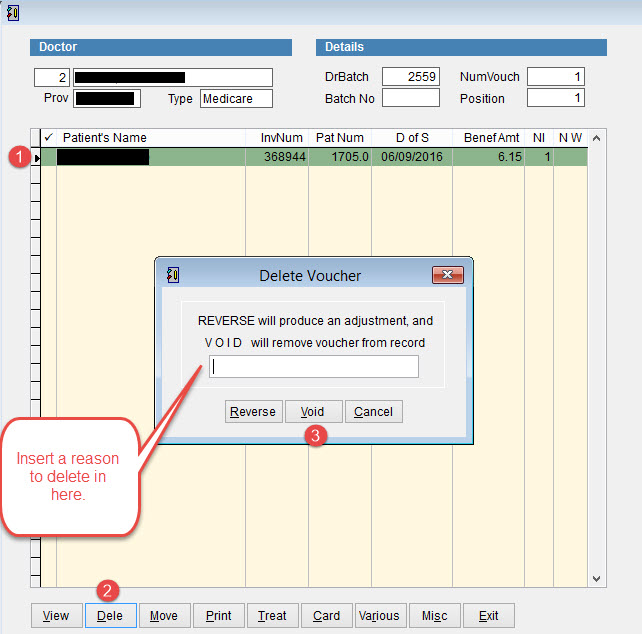
To Delete the claim, you will need to Move it out of the batch first, and then delete it from the Current Batch it is moved into. Please refer to the following screenshots:
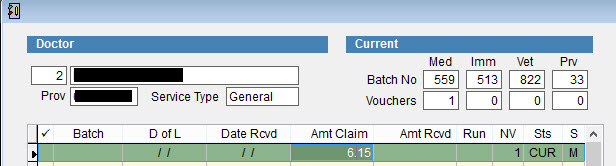
Once you have moved the claim out, you can go back to the main screen of the Batch Handler, and see a new “CUR” batch with the claim that was moved out.
View this batch and simply delete the patient inside as the following screenshot shows.